What Is A Partial Knee Replacement?
- A Partial Knee Replacement (PKR) is also called a “unicondylar knee replacement” (UKA), a partial knee “resurfacing” (PKR), and a partial knee “arthroplasty” (PKA). This is a surgical procedure that installs new surfaces replacing the old worn painful cartilage surfaces on the ends of the bones.
- Partial Knee replacements decrease or eliminate knee pain and swelling during weight bearing activity caused by the worn-out or damaged cartilage surfaces.
- Partial Knee Replacements can be performed in any of the three individual knee joint compartments that are painful and damaged.
- The compartments that can be replaced are:
- Medial (inner side and most common)
- Lateral (outer side and second most common)
- Patellofemoral (the kneecap compartment and least frequently performed)
- A “Bicompartmental” partial knee replacement is when a combination of two individual compartments are replaced at the same time, or added at a future surgery.
- The new replaced surfaces are called “implants” or “prosthesis” and they are usually made of cobalt chrome and titanium alloy metals, and a polyethylene plastic insert. These implants replace the damaged cartilage surfaces and the meniscus.
- Partial Knee Replacement with Dr. Buechel’s Mini-incision Mako Robotic assisted technique is dramatically less invasive, preserving all the healthy functioning structures of the knee.
- This is in contrast to a total knee replacement that removes and replaces all the surfaces in the knee joint at one time, even if some of the compartments are normal, or healthy and functioning properly.
- Partial knee replacements maintain all the healthy structures in the knee that are not damaged or degenerated. This means your ligaments in the middle of your knee called the ACL and PCL are allowed to remain and perform their normal functions providing stability and normal motions. The healthy compartments that are not affected by cartilage wear are all maintained.
- Partial knee replacements by Dr. Buechel are performed with a minimally invasive approach allowing rapid return to activity with significantly less pain. He uses a very small muscle sparing incision, Mako Robotic technology for consistently high precision, and he performs all of them as an outpatient procedure.

What Are The Keys To Successful Partial Knee Replacement?
- Choose an experienced orthopaedic partial knee surgeon to perform your surgery. One who has done several hundred at least in the compartment you are looking to replace.
- Choose an experienced surgeon to optimize and minimize your skin incision, be meticulous with the handling of your tissues, avoid cutting into the muscle, and provide a multilayered, cosmetic skin closure without using staples or sutures to remove if possible.
- Choose a surgeon who uses advanced technology to optimize the installation of you implants to your anatomy. This is critical to success.
- Optimizing implant alignment, sizing, tracking, ligament balance, and bone preparation are the installation keys to success and are possible using the Mako Robotic System on all cases.
- Choose a surgeon who uses Multi-Modal Pain management during and after the procedure to minimize the discomfort.
- Patients need to make the decision to optimize their health before and after their procedure and be dedicated to their recovery program to optimize their healing and rapid return to activity.
- Your surgeon should educate you why, or why not a partial knee replacement is best choice for you.
- Dr. Buechel will optimize the chance of your successful partial knee surgery with his 12-year Mako™ Robotic Partial Knee replacement experience on all his partial knees, his meticulous attention to all surgical details, and his comprehensive pre-surgery education and post-surgery protocols.

What Is A Mako Robotic Partial Knee Replacement?
A Mako™ Robotic Partial Knee Replacement Surgery is a partial knee replacement performed with a highly precise robotic installation system. This robotic system is one of the tools Dr. Buechel uses to precisely prepare the bones for the placement of the knee implants. He has been using this system for 12 years for partial knee replacements.
Pre-Operative Planning Tool
This system includes a highly evolved software package that allows Dr. Buechel to perform precision pre-operative planning of the intended implants’ sizes, alignments, and positions based on 3-Dimensional CT data of your hip, knee and ankle.
Intra-Operative Planning Tool
- Intra-operatively, Dr. Buechel adjusts the implants in the software to their final optimized locations from live knee bending and rotation information, optimized ligament tensioning, and cartilage or bone surface mapping data.
- The exact position of the implants is optimized based on ligament tension and gap analysis, limb alignment, implant tracking, and surface mapping data collected by the surgeon.
- Collecting and utilizing the data to optimize each person’s best implant position becomes the “Surgical-Art” of robotic knee replacement”.
Bone Preparation Tool
- The Mako™ Robotic-Arm is a precision cutting tool that cuts bone. It is used to create the shape on the bone to receive the implants according to the software plan.
- The robotic arm communicates with the planning software and the patient, with a camera system and tracking devices.
- Dr. Buechel helps moves the robot and the cutting tool to make the shape in the bone for the implants.
- The cutting tool follows the boundaries finalized in the software plan while providing more protection to the surrounding tissues.
- The Mako Partial Knee Replacement system provides precision bone preparation to 1mm and 1 degree.
Implant Position Verification Tool
Surgeons can use the Advanced Software tools included in the system to verify the correct impaction level and alignment prior to leaving the operating room.
Knee Replacement Implant System
- The Partial Knee Replacement implants included with the Mako Robotic System is the Restoris MCK™ Partial Knee.
- The software and robotic system are designed and validated only with the use of Restoris MCK™ Partial Knee Replacement implants.
- These implants are FDA approved. They have published that 90% or better successful results at the 10-year interval.
- The Implants are made of alloys of cobalt chrome and titanium and the plastics are made from polyethylene.
- Stryker provides their X3 Polyethylene for use with the Restoris MCK System which has shown excellent reduction in wear, which increases the life expectancy of the exchangeable insert.

What Is The Recovery Like For Dr. Buechel’s Mako Robotic Partial Knee Replacements?
- Dr. Buechel is an international expert and surgeon trainer for mini-incision Mako Robotic Partial Knee Replacement and has developed a system and techniques to help you recover rapidly and with less discomfort when he performs your partial knee replacement.
- The recovery for Dr. Buechel Medial Compartment Robotic Partial Knee Replacement surgery (the most common partial knee) is significantly less difficult than patients expect.
- Walking full weight bearing begins day one leaving the surgical center or hospital. You will start off with a cane, crutches or walker. You can eliminate any or all of these devices once you feel stable and confident with your balance. This is generally within the first week. But there is no rush and I want you to feel safe and use these devices until you feel ready and confident to discontinue them.
- The mild to moderate pain is generally limited to the first week. Swelling control is the main goal in the first 2 to 3 weeks.
- Once the swelling has resolved, the range of motion generally returns to the pre-op motion. Most patients by 6 weeks have all their pre-op motion back. By 3-6 months, many patients have increased their motion by 8-10 degrees.
- Physical therapy for robotic partial knee replacement surgery is not an aggressive painful process like most total knee replacement therapy can be. I start with simple patient home exercises the first week to allow for wound stabilization and swelling reduction.
- Then I begin formal physical therapy the second week for most patients focused on improving the quadriceps strength and proper return of a normal, or near-normal gait cycle.
- Stationary bike exercise can begin right away using the non-operative leg only, to get your cardiac conditioning going and release the good endorphins into your system. Starting week 3, you can use both legs on the bicycle. This is recommended to give your skin and inner tissues time to start to heal together before over stressing the sutures underneath.
- I limit high impact exercises like jumping or running, and high torque twisting like a strong golf swing and singles tennis until the 8-week mark. Not that you cannot do it, but to allow the bone to stabilize where the tracking pins were inserted during your surgery, to reduce the risk of a bone fracture at the pin sites.
- Driving is generally okay by the end of the first week for most patients with the understanding that you are not allowed to drive ever if you are taking narcotic pain medication. You should test yourself in your driveway first making sure you can step hard on the break for safety before you travel any distance.
- Lateral Compartment Partial Knee Replacement patients often have a similar recovery to the medial side patients, but sometimes it takes a month or two longer for the lateral side patients to get to the higher-level exercise activities than the medial side patients take.
- Patellofemoral Compartment Partial Knee Replacement patients in general take longer than the Medial and Lateral compartment partial knee replacement patients to recover fully. There is more post-operative soreness and stiffness in the front of the knee surgery recovery. Therapy is more aggressive to get the range of motion and strength to return after patellofemoral partial knee replacement, but this is still far less difficult than a total knee replacement recovery, if only the anterior compartment is damaged.

What Is The Recovery Like For Dr. Buechel’s Mako Robotic Partial Knee Replacements?
- Dr. Buechel has developed a comprehensive pain control process for his Robotic Partial Knee Replacement patients to make the procedure and recovery as comfortable as possible.
- The first 2 days are generally very comfortable because of the nerve blocks done at the time of the procedure.
- Days 3 through 6 are the days that can be uncomfortable for some, as the blocks start to wear off, but not anything like total knee replacement pain can be.
- After the first week, most patients will not be taking any narcotic pain medication and ibuprofen and acetaminophen generally is all that is needed.
- By two weeks most patients have 85% of the swelling gone which makes it easier to start getting the bending to return as expected.
- Also, at two weeks, most patients are only taking over the counter medications as needed for discomfort and do not require narcotics.
- Dr. Buechel’s pain control program includes all the following:
What are some of the things Dr. Buechel does to significantly lessen your pain during your recovery?
- He has developed several techniques using special instruments and a stabilizing leg holder that allows him to make a very small incision, put very little stretch on your skin and tissues, and still have great visibility to precisely install your implants with minimal tissue injury.
- He has his anesthesiologist provide you with a spinal anesthesia if possible and two blocks that give you great pain control after the surgery for 36 to 48 hours. He also places local anesthetic into the wound to provide you with even more pain control.
- He provides you with a knee cooling sleeve after surgery to reduce pain and swelling.
- Using the ice machine, most patients only require ibuprofen and acetaminophen after surgery. Some patients will take a few low-level narcotic pills for a few days the first week after surgery.
- Dr. Buechel will place a sports compression sleeve on your leg in the office the day after surgery which reduces swelling and pain.
- Elevation is an extremely important part of the protocol along with the compression sleeve to reduced swelling, which reduces pain.
- Dr. Buechel does not use a tourniquet that squeezes your thigh and stops blood flow during surgery, which will dramatically reduce the pain after surgery and reduces your blood clot risk.
- A commonly used IV steroid medicine is used by the anesthesia team to reduce nausea which also helps to reduce swelling after surgery and provide some increased pain control.
- We have found that avoiding aggressive physical therapy early in the first week allows the wound to seal and swelling to reduce.
- Walking and simple exercises are all that is needed the first week.

What is the follow up care like for a Robotic Partial Knee Replacement Surgery?
- Patients return to the office the day after partial knee surgery
- The surgical dressing is changed if necessary.
- New dressings supplies are provided to change the dressings at home once a week for 3 weeks. (you may shower with or without the dressing)
- A compression Sports Knee sleeve is applied from the ankle to the groin to help with swelling, provide support, and reduce discomfort.
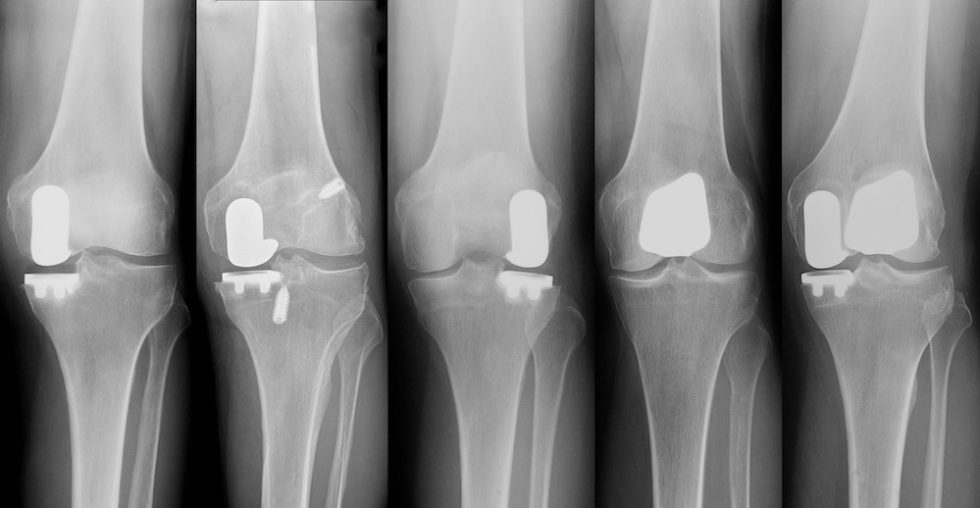
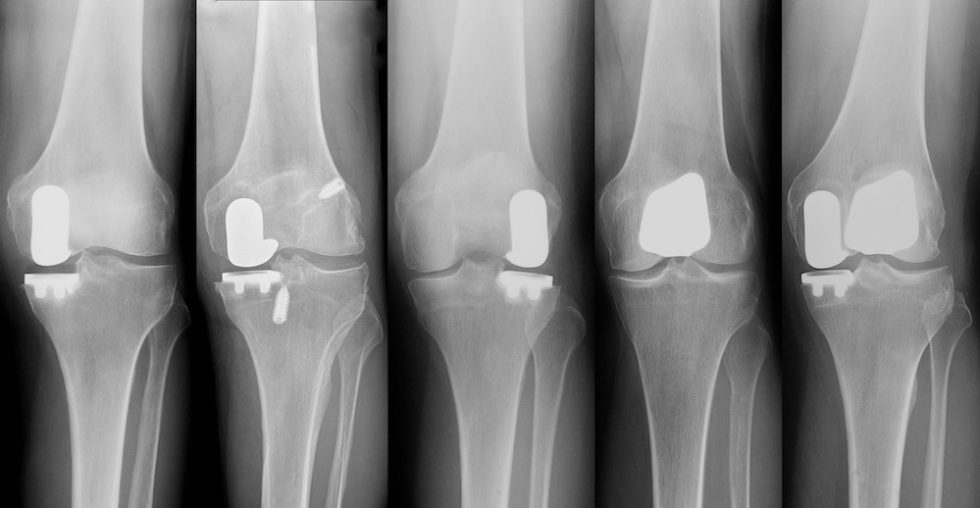
- Your Post-Operative X-rays will be scheduled, obtained and reviewed with you in the office on the large format screens digitally.
- Patients can return home if they are traveling to New York for their surgery generally in 1-2 days if needed. Many patients will fly home from New York within just a few days of their procedure.
- We maintain close contact with you in the early recovery phase to make sure you feel comfortable and all your concerns are addressed.
- We like to see you back if possible, in 4-6 weeks after surgery, or check in via our Virtual Consultation platform using Doctor.com.
- We like to have another contact at 6 months after surgery which is another check-in milestone when we like to hear from you.
- Annually we like to have a check-in and x-rays of the operative knee to ensure everything is as desired.

What are The Indications that someone may require Robotic Partial Knee Replacement Surgery?
Deciding to have a partial knee replacement requires that your clinical history, physical symptoms, physical exam and imaging (x-rays and sometimes MRIs) all point towards partial knee replacement.
The synthesis of this information requires a skilled partial knee surgeon, like Dr. Buechel, to listen, then ask the right questions, perform a proper partial knee exam, and understand the imaging. Once Dr. Buechel has all of this information, he will confirm with you where the problems are, and provide you with the correct recommendations.
Each compartment of the knee has its own specific indications as to whether or not a partial knee is a good option. You may review these indications on our webpages designated specifically for each compartment for more detailed information.
These pages can bee see by clicking on the hyperlinks to our specific pages here:

When is the right time to have a Partial Knee Replacement?
- The decision on when to have your partial knee replacement performed is quite straight forward.
- It starts by having a proper exam and imaging that confirms you’re a candidate for the procedure.
- Once you know you’re a good candidate, the timing is really up to you.
- It is never an emergency to have the procedure.
- The only problem with delay is a reduction in your quality of life, and continued pain.
- Therefore, when the pain is no longer tolerable, when your quality-of-life decreases, or when you can’t enjoy the things you like to because of your knee pain, then this would be the right time to move forward with your procedure.

What Dr. Buechel does to improve your Partial Knee Outcomes?
There are many things that a surgeon must manage and many choices to be made to ensure an optimal outcome for every patient. We have provided a list of these things that Dr. Buechel manages during and after your surgery to enhance your procedure, reduce risks of complications, and help in your recovery. This is an extensive list but does not cover all the things that are done to try to get you the best outcome possible.
EXPOSURE AND SAFETY
- Dr. Buechel uses a Specialized Padded leg holder designed to support your leg safely during the partial knee procedure (IMP Leg Holder)
INFECTION CONTROL
- Dr. Buechel wears a Joint Replacement Space Suit with lighted helmet for optimal visualization and protection
- Adhesive Drapes are used to seal skin during surgery
- Antibiotics are in the Bone Cement
- Antibiotics are given to you in your IV
- Preoperative and postoperative Nutritional Supplementation is recommended to optimize your healing and immune system
MUSCLE AVOIDING INCISION
- Dr. Buechel precisely draws the anatomy for optimal incision size and position
- 2-3-inch skin incision is used for most medial partial knee procedures
- Avoiding Muscle allows for faster return to activity during the recovery process
BLOOD LOSS CONTROL
- The medicine Tranexamic Acid is given intravenously to reduce blood loss
- Lidocaine 1% with Epinephrine is injected into the incisions to reduce bleeding
- Meticulous hemostasis during exposure reduces blood loss
- No Tourniquet is needed to control bleeding
- Orthobiologics Application into joint and would closure reduces bleeding
- Proper knee positioning and use of the leg positioner during surgery reduces blood loss.
ANESTHESIA
- A multimodal approach to your pain control provides an optimal recovery
- Spinal Anesthesia is recommended, General Anesthesia is just fine if better for you.
- Regional pain block #1: I-PACK Block
- Regional pain block #2: Adductor Canal Block
- Periarticular Local Block: Marcaine, Ketorolac, Morphine
BLOOD CLOT REDUCTION
- No Tourniquet
- No instruments in the canals of the bones to cause emboli
- Spinal Anesthesia reduces blood clot risk
- Walking within hours of the surgery reduces clot risk
- Aspirin 81mg twice a day for 4 weeks
- Efficient surgical process reduces risk
- A compression Sports sleeve is used after surgery for 4-6 weeks
SUTURE CHOICES
- Micro-barbed sutures
- Avoids knot abscesses
- Antibacterial material lowers infection risk
- Provides a Watertight closure
SKIN ADHESIVES:
- Dermabond Skin Adhesive seals the skin edges
- Allows Showering the Day after surgery
- Provides a Barrier to Infection
- Provides better scar appearance
- Removes easily at 3 weeks
BIOLOGIC TREATMENTS
- Orthobiologics Application into the knee joint and would closure enhances healing and the cellular repair process.
SKIN DRESSINGS
- Silicone Boarder Dressings are used
- Reduces skin irritation
- Waterproof for showering
- Remain on for 5-7 days
- Anti-bacterial
- Protects the skin glue from clothing rubbing it off
COLD THERAPY WRAP / COOLING DEVICES:
- Wear continuously as tolerated after surgery
- Reduces swelling
- Reduces pain
- Reduces medication requirements
- Improve motion
- Commonly used for 4-6 weeks daily to optimize swelling reduction early
COMPRESSION SLEEVE:
- We provide a Reparel Compression Knee Sleeve after surgery
- These Reduce swelling
- Provides comfort/support
- Improves blood flow
- Used for 4-6 weeks to optimize recovery
MEDICATIONS
- Decadron IV Pre-incision & Post Op given in Operating room (Steroid to reduce
inflammation)
- Aspirin 81mg twice a day for 4 weeks (Reduce Blood Clot risk)(Pain reducer)
- Acetaminophen (Pain and Inflammation reduction post op) as needed
- Ibuprofen (Pain and Inflammation reduction post op) as needed
- Hydrocodone (Moderate pain reduction medication, if needed)
INSTRUMENTS
- Specialized custom retractors and tools are used to minimize tissue injury
- Specialized instruments to optimally prepare the bone and soft tissue surfaces
- Dr. Buechel is gentle with tissue retraction to optimize wound healing
PHYSICAL THERAPY
- We provide a comprehensive post op therapy program for home and your therapist
- Gentle therapy starts the day of surgery
- No high impact activity 6-8 weeks
NUTRITIONAL SUPPORT
- Protein Supplementation is recommended to enhance wound healing
- Vitamin C: (to enhance wound healing and infection reduction)
- Probiotics: (to support your microbiome to optimize healing and to minimize the
negative the effects of the antibiotics on your GI Tract)
Contact Us
The simplest way to schedule an appointment with Dr. Buechel is to call us directly at 212-308-3089. We will schedule an In-Office Appointment or Virtual Consultation for your first encounter. Our practice hours are Monday through Friday, 9:00 AM to 5:00 PM.
If you don’t have the time to call or it is just easier, you can contact our staff with a quick email at info@RoboticJointCenter.com and we will email you back within 24-48 hours. If you wish, let us know in your email and we can also call you back at a designated phone number you provide.