PARTIAL KNEE REPLACEMENT:MEDIAL COMPARTMENT
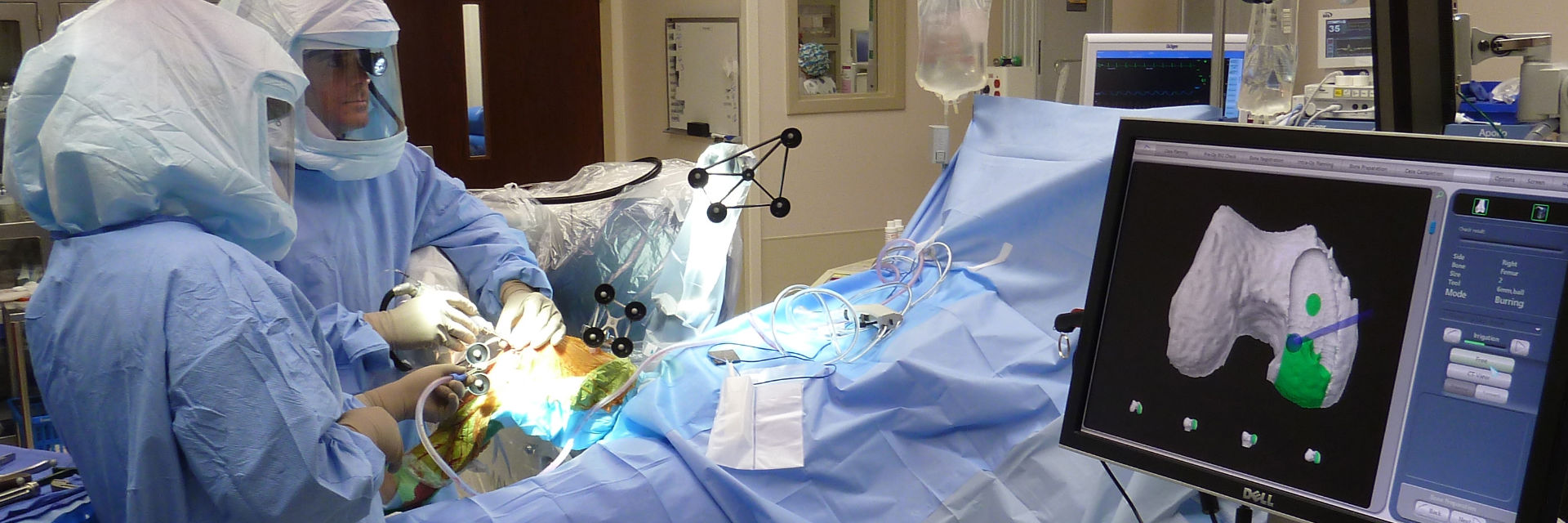
MAKO ROBOTIC-ARM ASSISTED
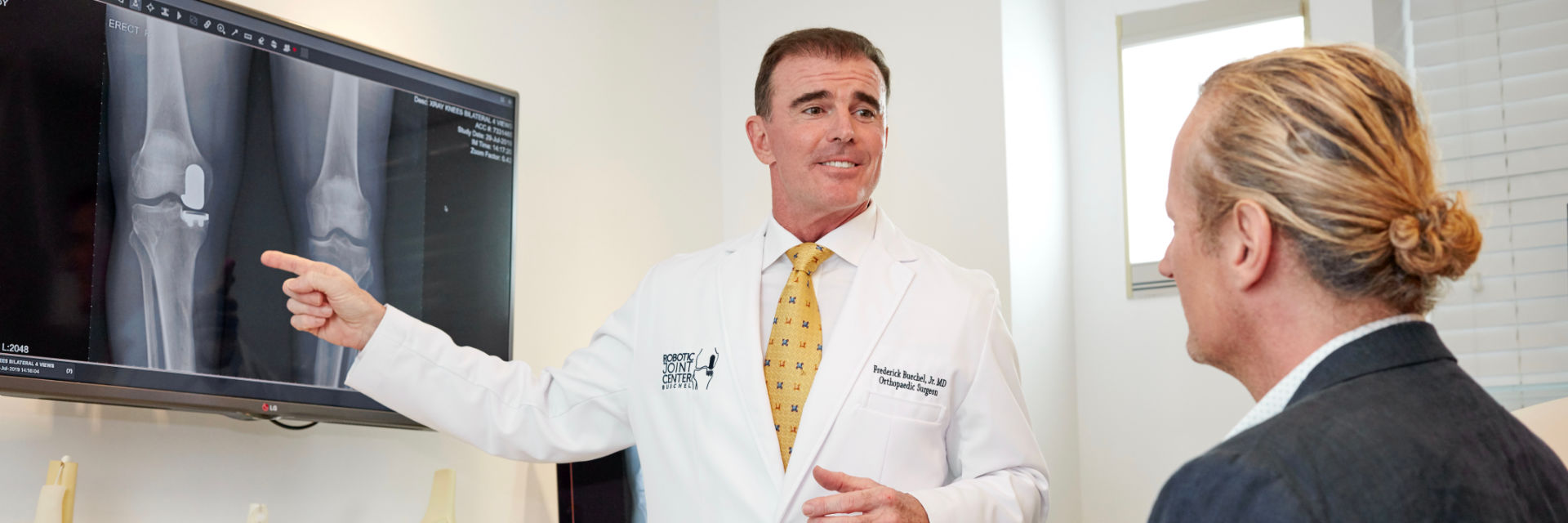
Dr. Frederick F. Buechel, Jr. M.D. is a Super-Specialist in Partial Knee Replacement with Robotics. He is one of the worlds authorities on Mako Robotic Partial Knee Replacement and has performed over 1,500 Medial Mako Robotic Assisted Partial Knee Replacements in the USA and internationally. He is a sought-after knee surgeon for his Outpatient, Mini-Incision, Tourniquet-Free, Mako Robotic Assisted Partial Knee Replacement.
Dr. Frederick F. Buechel, Jr. M.D. is a Board-Certified Orthopaedic Surgeon, fellowship-trained in Joint Reconstruction from the University of Pennsylvania in Knee & Hip Replacement. He is the founder of the Robotic Joint Center in New York and Taiwan. Former Chairman of the Department of Surgery and Chief of Orthopaedics in Naples, Florida. He is a Stryker International Mako Partial & Total Knee Instructor and has launched programs in the USA and over 10 countries, performing the first Mako Partial Knees in Australia, Singapore, Taiwan, Hong Kong, Greece, Thailand, Vietnam, and China,
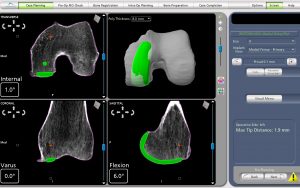
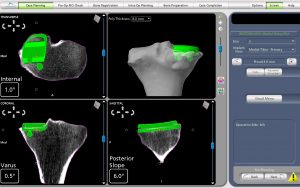
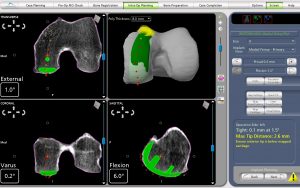
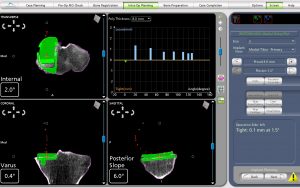
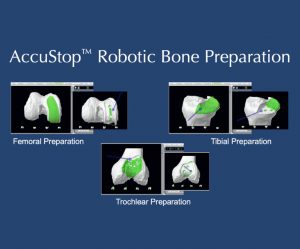
“The Details Matter”! Dr. Buechel is a meticulous partial knee replacement orthopaedic surgeon and is a master of medial partial knee replacement techniques that optimize patients’ outcomes. He has been using the Mako robotic system for over 12 years for his partial knees to ensure each patient’s knee installation is optimized. The robotic system allows Dr. Buechel to customize each patient’s installation to their specific anatomy and soft tissue tensions with precision robotic bone preparation, and software assisted knee motion optimization.
Contact Us Today!
Have Dr. Buechel Help End your Knee Pain,
and Get you Back to an Active Lifestyle