Osteoarthritis
What Is Osteoarthritis?
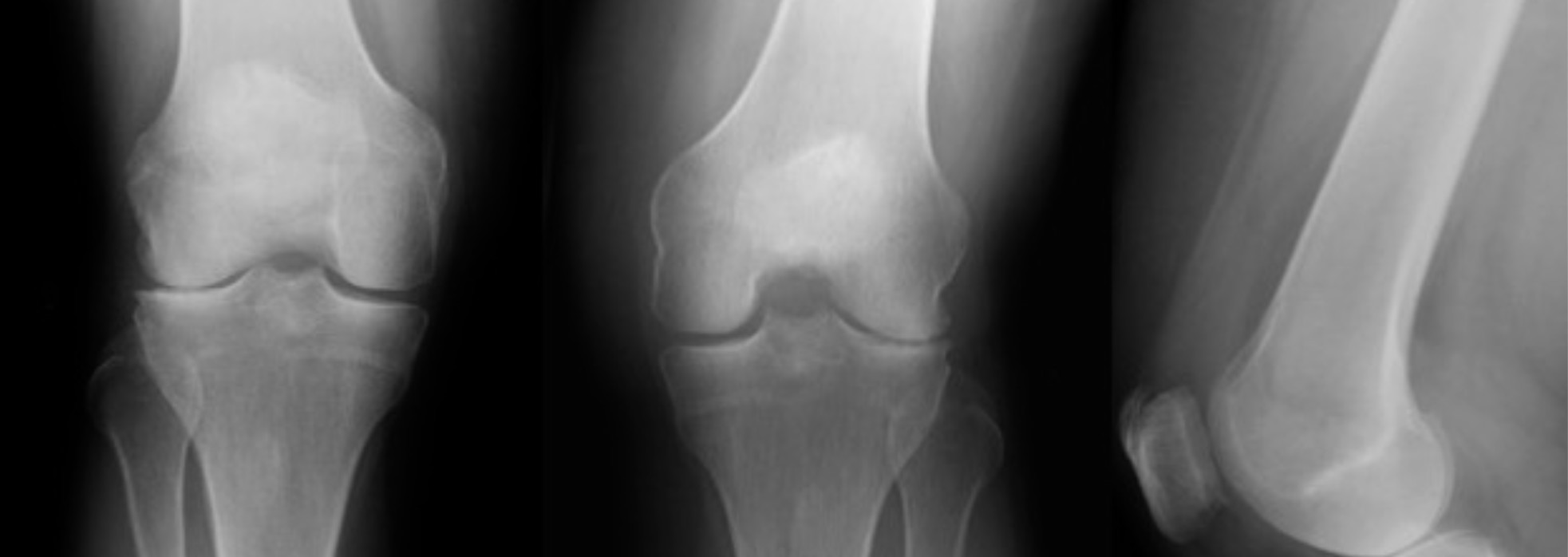
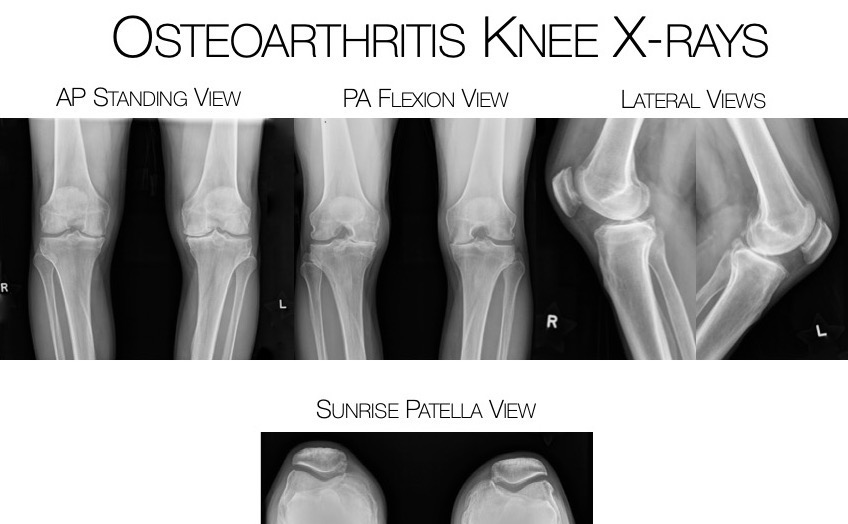
Osteoarthritis is the most common form of arthritis. “Osteoarthritis” means joint inflammation from a degenerative condition or wear and tear of the knee joint cartilage. This condition can occur as the result of a traumatic injury to the knee or, from a genetic predisposition to cartilage degeneration.
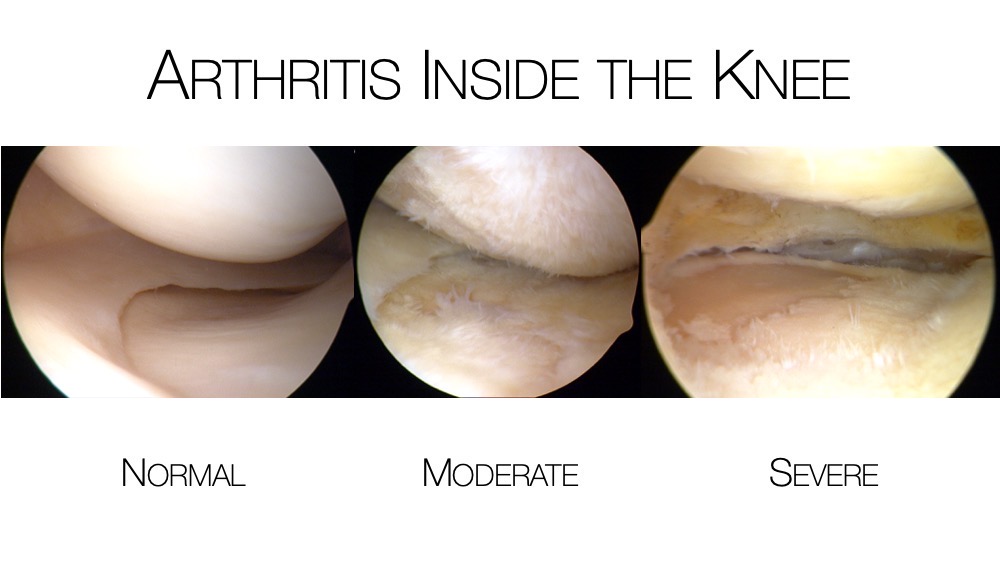
This process can begin with cartilage softening which can lead to fraying and fissuring of the surface cartilage, ultimately progressing until it is completely worn from the bone. Bone spurs (osteophytes) can form as the pressure on the bones increase and the bone tries to spread the force over a larger surface area, creating more bone.
Synovial fluid production often increases to lubricate the worn surfaces and begins to fill the knee compartment causing swelling, pain, and reduced range of motion.