What Is Osteonecrosis of the Knee?
Osteonecrosis means “bone death”. The bone cells can die due to blood flow reduction, lack of oxygen to the cells, and the bone then begins to cause pain. Pain can occur at rest and with weight bearing, unlike osteoarthritis pain that occurs mostly with weight bearing, and is relieved with rest.
Osteonecrosis can occur in any bone, but it is commonly seen in the knee and hip joints. In the knee, osteonecrosis can occur in the end of the femur or the top of the tibia bone. It can occur in just one bone and on just one side of the bone, but it can also occur in both bones and throughout the entire end of the bones. Bone death can start off in a small area and can progress to a large area of bone. Sometimes the process stops early, and the pain can go away.
In the early stages the condition is not seen on x-ray but can be seen with MRI. In these early phases, there are some potential non-joint replacement options that attempt to stop the progression of the process. As the osteonecrosis process worsens, the cartilage surfaces can collapse into the dead bone area causing more significant pain and disability. Once the process goes on to joint surface collapse, joint replacement is the only solution to relieve the pain and restore function.
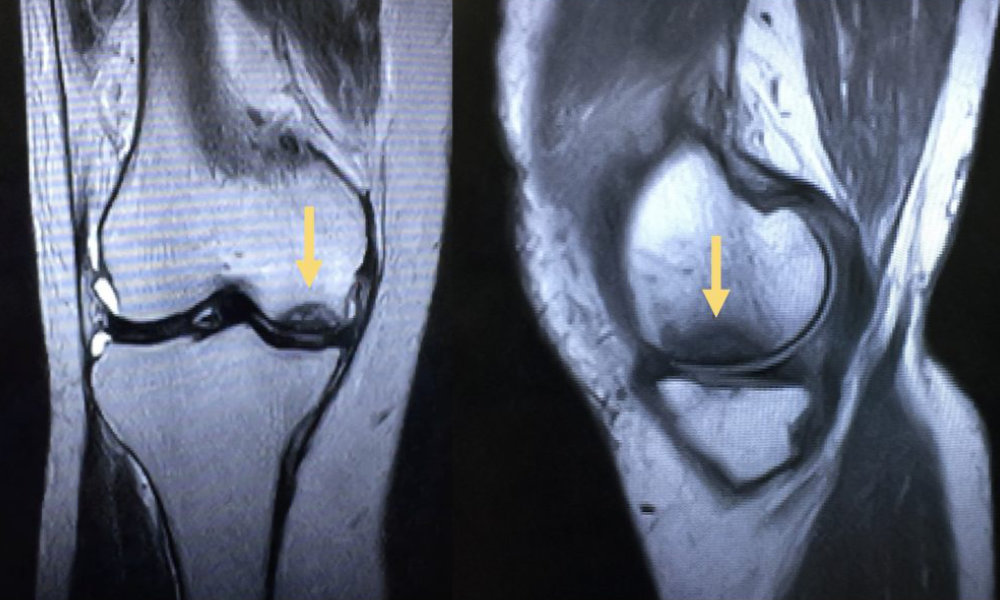
MRI View
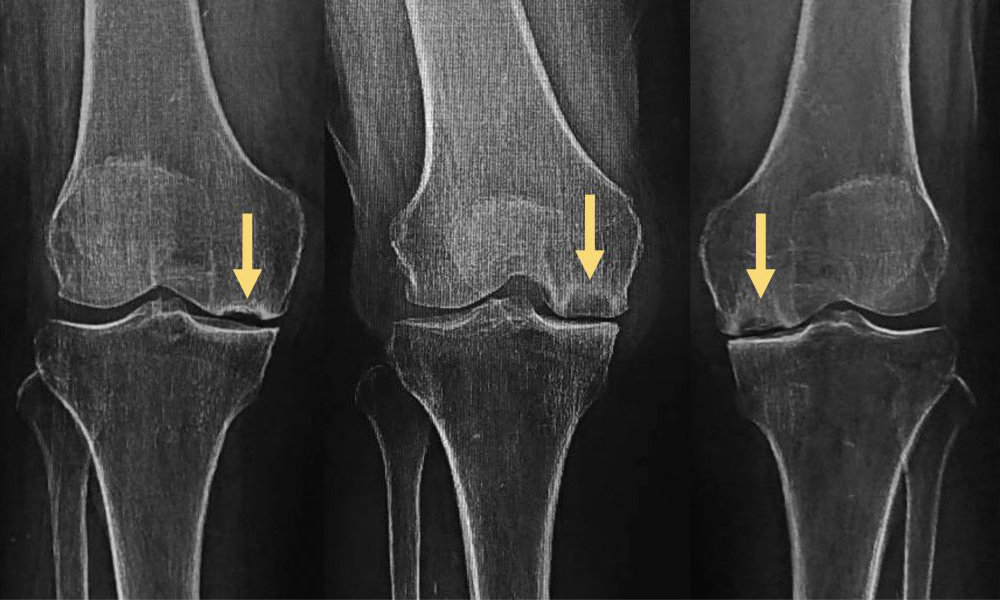
X-ray View