What Is A Total Knee Replacement Surgery?
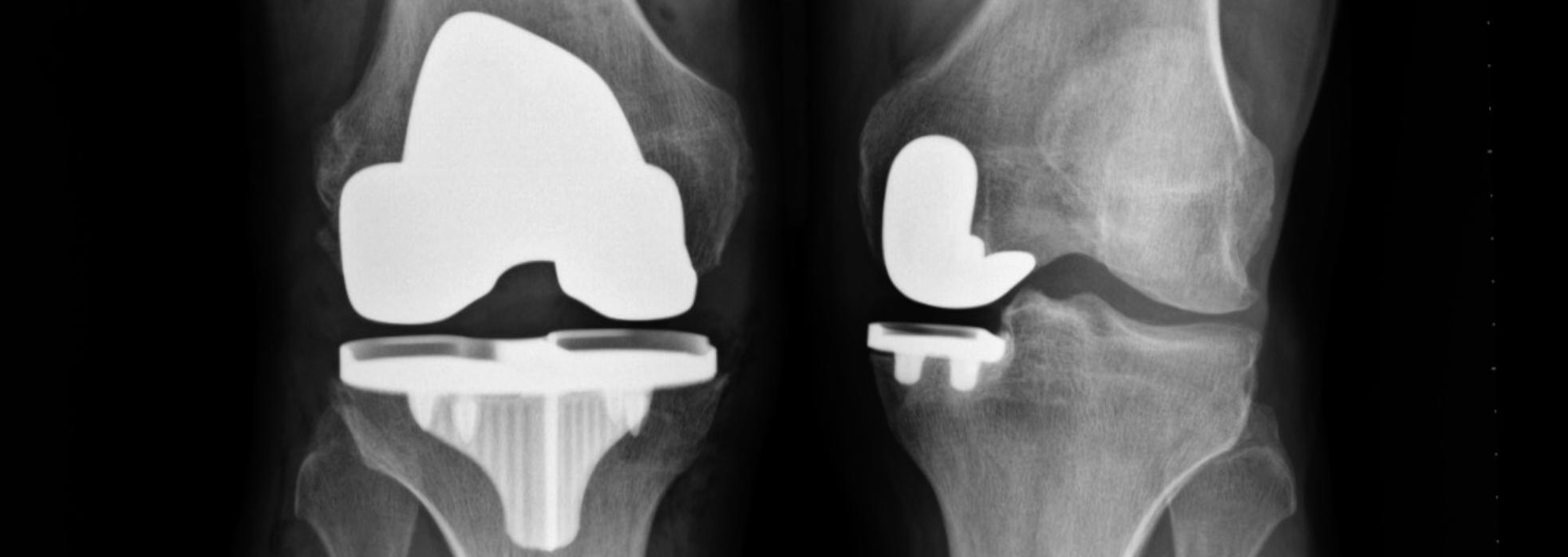
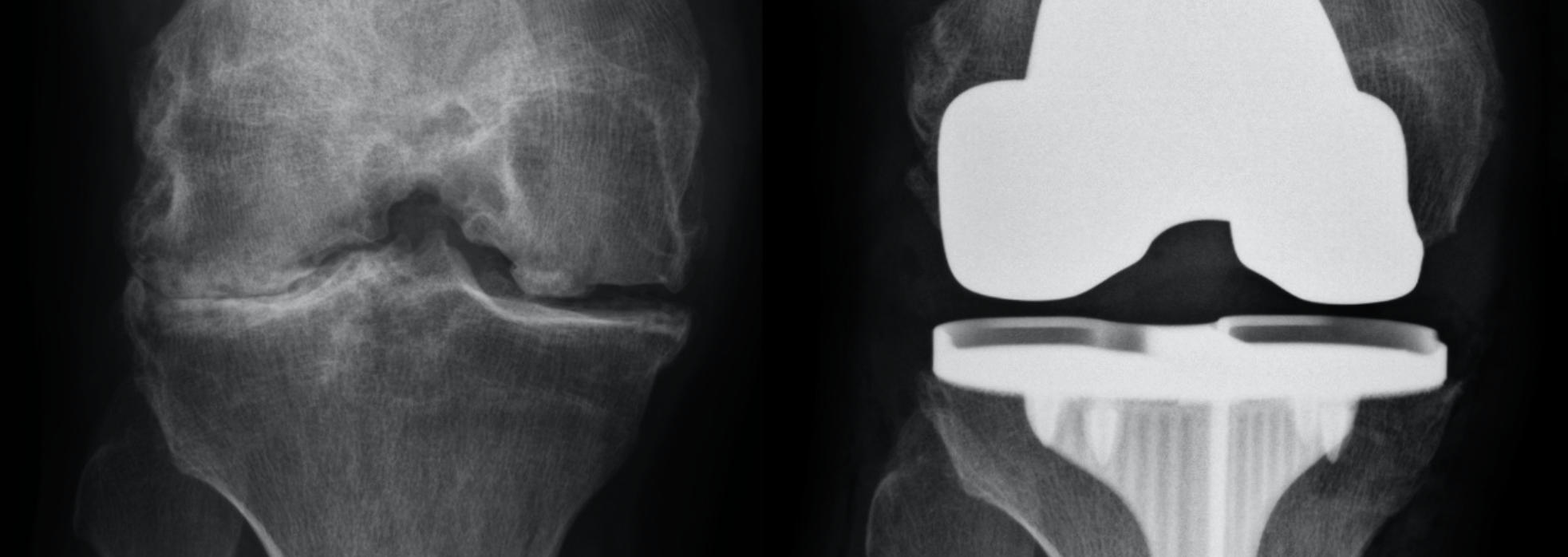
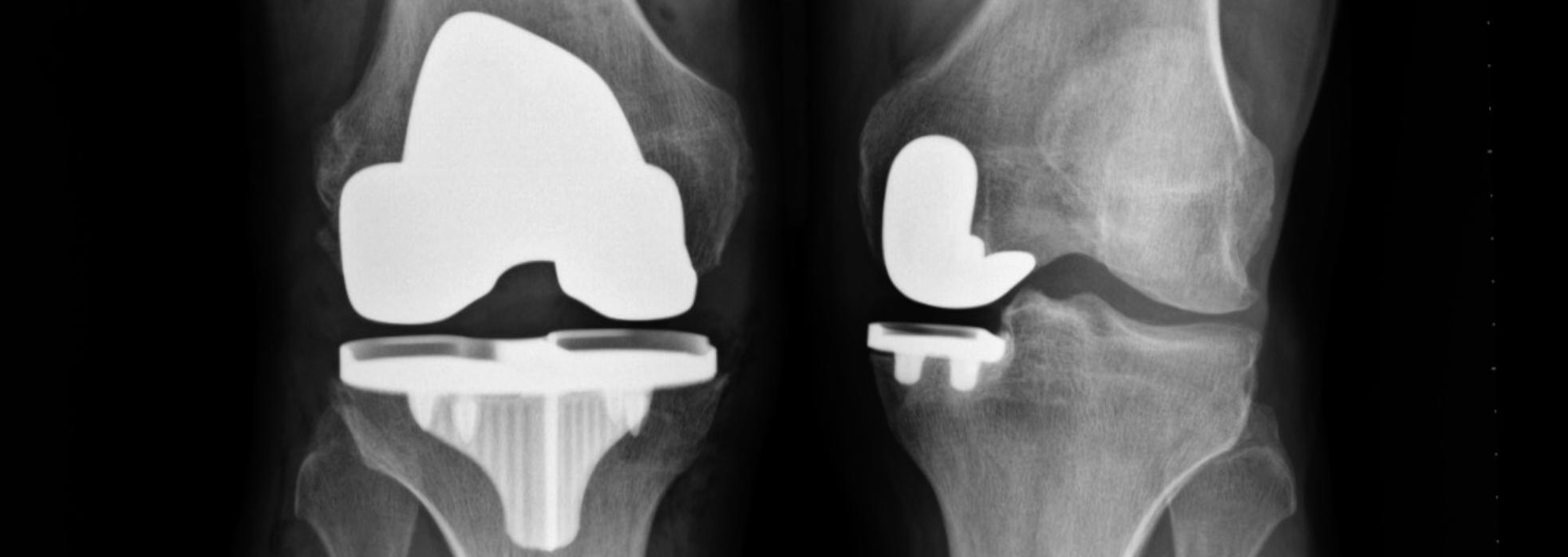
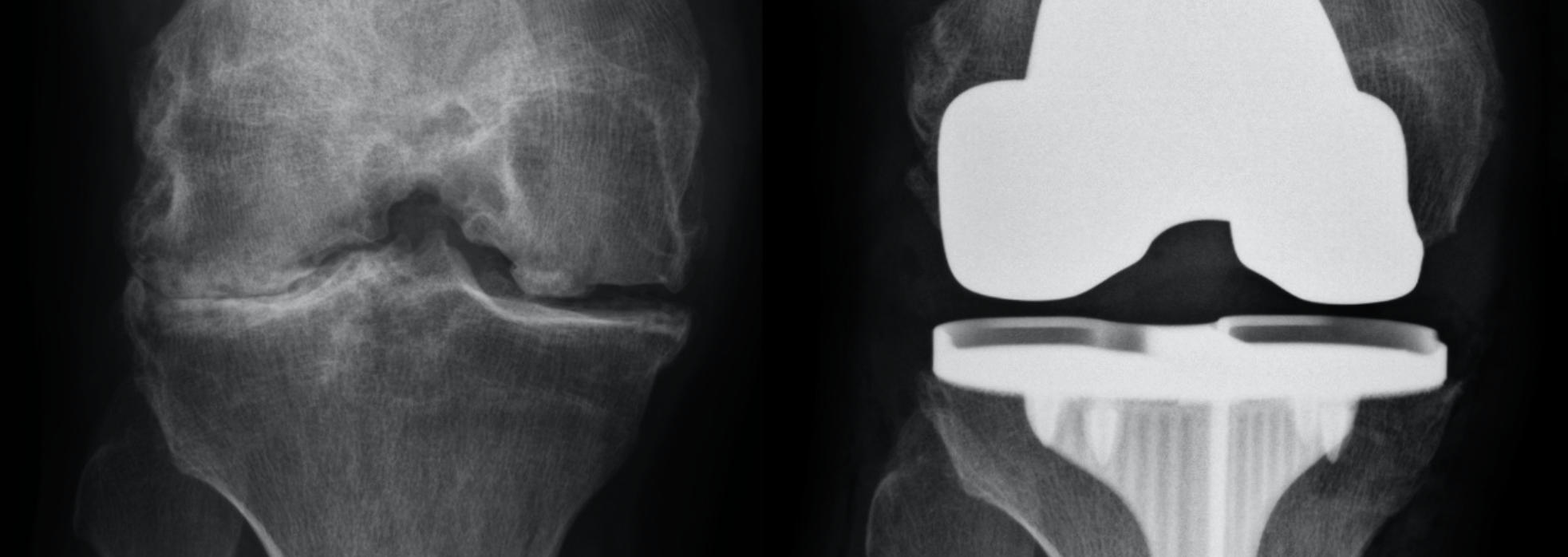
A Total Knee Replacement, “TKR” (also called Total Knee Arthroplasty, “TKA”) is performed to replace the worn down or damaged knee joint surfaces in all three compartments of the knee that are causing pain with weight bearing activity. The damaged joint surfaces on the end of the femur (thigh bone) and top of the tibia (shin bone) are replaced with new surfaces called implants, usually made of metal alloys of cobalt chrome and titanium, and a ultra-high molecular weight polyethylene plastic insert bearing. The insert is installed between the metal parts and acts as the cushion, creating a low friction joint surface.
The surgical procedure is performed through a straight skin incision on the front of the knee and a deep incision entering into the joint that allows the ends of the femur, tibia and kneecap to be exposed. This allows all 3 compartments, the medial on the inside, the lateral on the outside, and patellofemoral compartment in the front to be replaced with the new knee replacement implants.
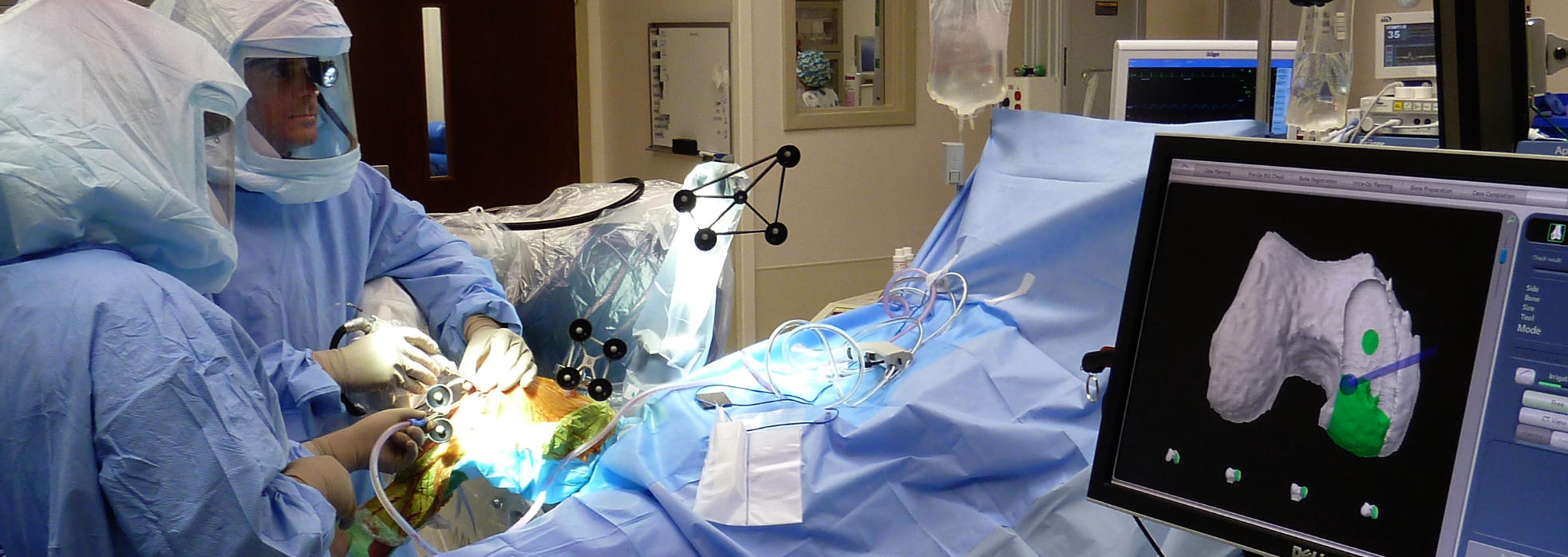
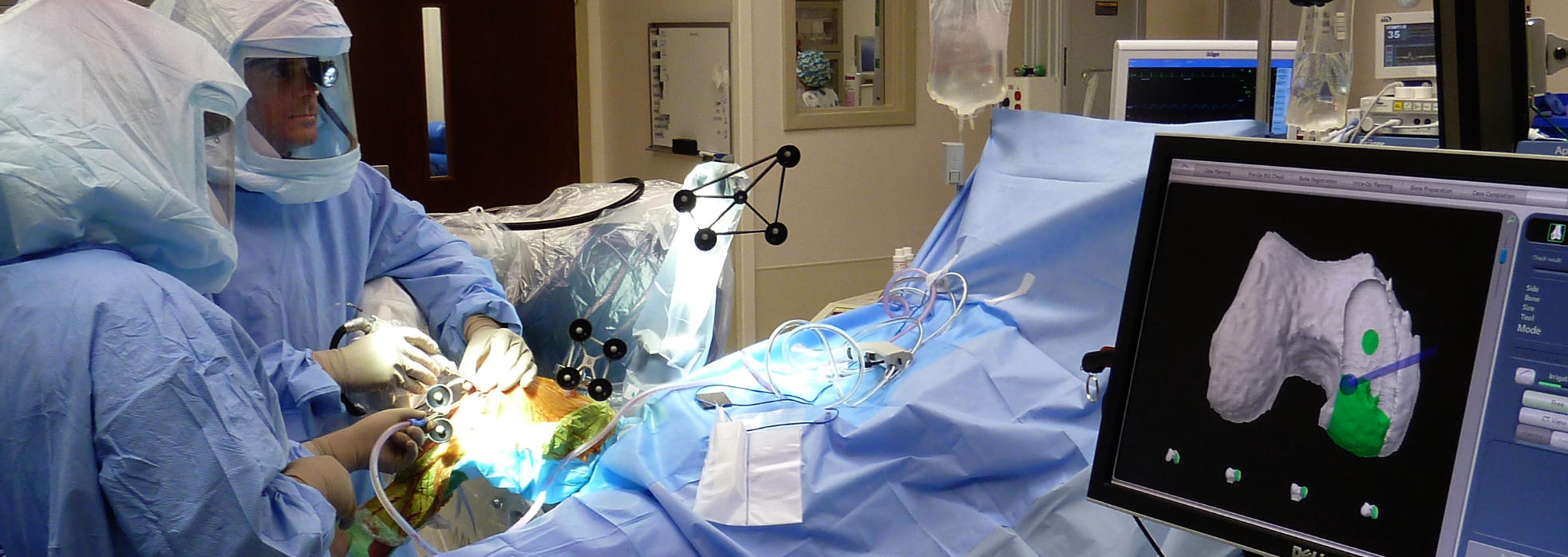
In order to place the new implants on the bone surfaces, the worn bone surfaces have to be cut and shaped to accept the implants properly. The proper sizing, position, rotation and alignment of the implants for each individual must be carefully performed to provide the optimal outcome, feel, pain relief, range of motion, alignment and longevity of the new knee replacement. This process can be performed with conventional cutting guides, tools and saws. Or, it can be done with highly advanced technology like the Mako™ Robotic Total Knee Installation System that Dr. Buechel uses.
Once the bone is properly prepared to receive the implant, the parts are attached to the bones. Implants can be attached to the bone either with bone cement, or without cement, called cement-less. Cement-less implants have a special surface that allows the bone to grow into the metal, biologically attaching the implant. Cemented implants use polymethylmethacrylate bone cement which acts as a grout to attach the implants to the bone surfaces and hardens within minutes once mixed during the procedure. Both fixation options have similar long term success rates.
Once the surgery is completed, patients either go home, stay in the hospital for a night or two, or go to a rehabilitation facility based on the surgeon’s technique, their medical conditions, pain control and function. Total knee replacement patients will undergo physical therapy after their surgery for several months working on range of motion and strengthening, until they are able to get back to their own exercise programs.
Knee replacements done properly and without complications, can last several decades and provide significant pain relief and function, returning patients back to an active lifestyle.

Total Knee Replacement vs. Resurfacing vs. Arthroplasty
There are several terms that are used interchangeably to describe knee replacement surgeries. The synonymous names include total knee replacement “TKR”, total knee resurfacing “TKR”, and total knee arthroplasty “TKA”. The term resurfacing is sometimes more commonly associated with partial knee replacement, but it can be used to describe both total and partial knee replacement.
Partial Knee Replacement vs. Total Knee Replacement
A Total Knee Replacement is performed to replace the worn down or damaged knee joint surfaces in all three compartments of the knee that are causing pain with weight bearing activity. Patients for total knee replacement usually complain of pain throughout the entire knee. Total Knee replacements are able to fix knees that are more damaged, have severe deformities, have ligament damage or loss, are damaged due to inflammatory arthritis like “rheumatoid arthritis”, have been previously replaced and have failed or loosened, and for patients that are severely obese.
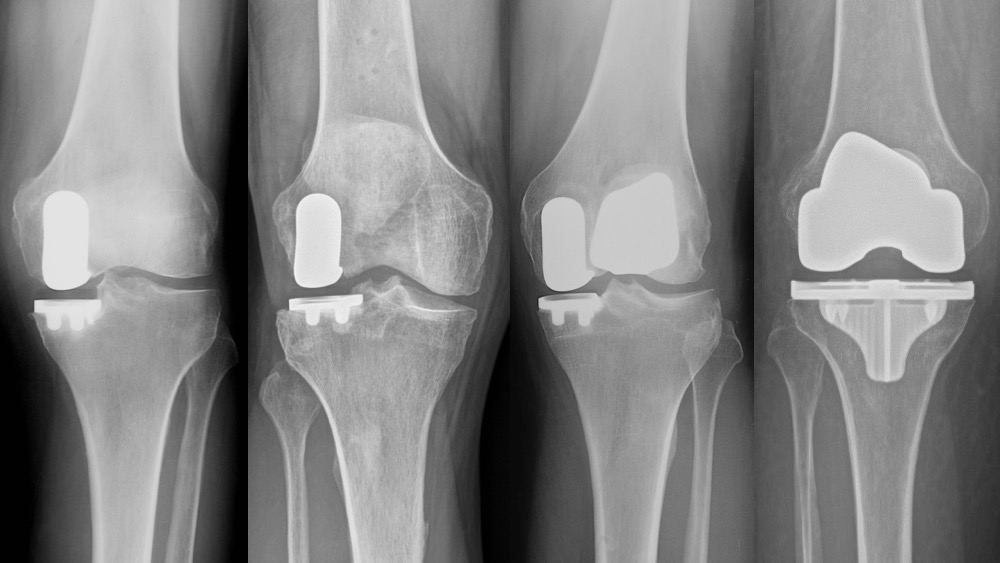
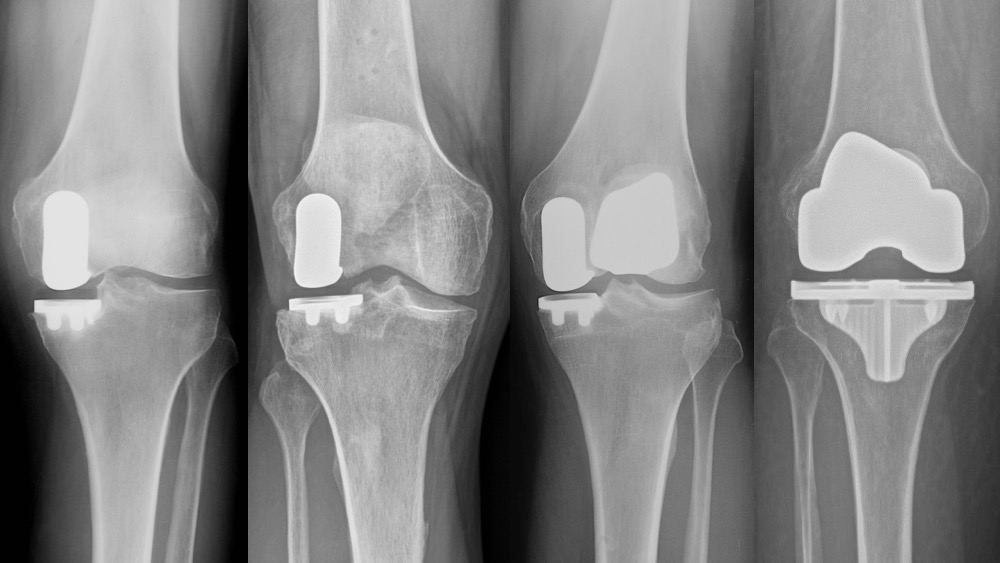
Partial Knee Replacement is performed to replace one or two of the three compartments of the knee joint and maintains the healthy compartments and ligaments that may not be damaged or deteriorated, allowing more normal function and motion that a total knee replacement. Partial knee replacement is much less invasive and has an easier recovery than total knee replacement. Patients for partial knee will generally complain of pain on one side of the knee or the other (inner side “medial”, or outer side “lateral”), or just under the kneecap, “patellofemoral”. Partial knee replacement should be considered first, and only if it is contraindicated should total knee replacement be chosen. Partial knee replacement is not for inflammatory arthritis, it is for osteoarthritis, osteonecrosis, or post-injury arthritis knee pain. In general, it is not for severe deformities, should be performed on patients with intact and stable ligaments (but sometimes is okay if the ACL is not present), and it is not possible after a total knee replacement has already been done.
Dr. Buechel looks at each patients situation individually before deciding on partial knee replacement or total knee replacement. The preferred procedure for Dr. Buechel to perform is partial knee replacement first, if indicated. (See Partial Knee Replacement Indications) When looked at critically, probably 50% of patients or more can benefit from partial knee replacement instead of total knee replacement, in the hands of an experienced partial knee surgeon. This is why getting an opinion from a very experienced partial and total knee surgeon is important to truly know your options.
Most surgeons perform less than 10 partial knee replacements a year and will tend to recommend a total knee for their patients, even if they could have a partial knee replacement because this is more comfortable for them to perform. A well done total knee is a great fix restoring function and decreasing pain, but a well done properly indicated partial knee feels better and more natural than a total knee.
This is why having your knee evaluate by Dr. Buechel who has done more than 1,500 robotic partial knee replacements as well as being an expert total knee replacement surgeon is beneficial. A review of your history, a physical exam and proper recent x-rays are generally all that is needed for Dr. Buechel to help you understand which option is best for you.

Is Total Robotic Knee Replacement Considered A Virtual Knee Surgery?
Mako™ Robotic Partial & Total Knee Replacement is not virtual surgery like the well known DeVinci robotic surgery system where the surgeon sits at a console on the side of the operating room controlling the Robot above the patient. The Mako Robotic Total Knee Replacement System uses a CAT scan image to extremely accurately plan and customize the implant placement for each individual. The Mako Robotic Arm is held by the surgeon and the cutting tool at the end of the arm is guided by the surgeon across the bone surface, while the robot controls the boundaries of the cutting tool, preventing cutting outside the boundary. The software is used to plan, adjust and confirm the implants installation is performed properly. The surgeon is in full control of the planning, bone preparation and implant installation during the entire procedure. The robot is only an advanced tool that communicates with the software to ensure the bone cuts are precise and safe as it protects the surrounding soft tissues from harm during the surgery. This safety feature is one of the special features of the Mako Total Knee Robotic System.
Why Is A Total Knee Replacement Surgery Performed?
The main indication for requiring a total knee replacement is when a person has global knee pain with weight-bearing activity that is limiting function and reducing quality of life from osteoarthritis, rheumatoid arthritis, osteonecrosis, or traumatic arthritis from a prior knee injury like a meniscus tear, or fracture. Patients should have tried conservative treatments first, and no longer are responding to non-surgical treatment. Patients with severe angular and fixed deformities are better treated with total knee replacement over partial knee replacement, in most cases.

How Do You Prepare For Total Knee Replacement?
Patients that are considering undergoing knee replacement surgery can do several things to prepare for their surgery. Some are required, others can optimize your outcome.
- You should prepare your home for your arrival after surgery making food available and removing any objects that could be tripping hazards.
- You should contact your insurance company to personally understand your benefits (each plan is different).
- If you are working, you should discuss your plans with work, get any paperwork ready they require, and prepare for your time off and return.
All patients should have a medical checkup by their family physician or medical doctor to clear you for surgery and provide medical recommendations.
If there are any special medical conditions you have, a specialist may be required to check you out and provide recommendations for your management before, and after your surgery. Specialists that might get involved in your surgery preparation could be:
- cardiologists if you have heart conditions
- nephrologists if you have kidney conditions
- hematologists if you have blood conditions
To optimize your health:
- Eat well
- Get enough protein
- Take appropriate vitamin supplements and discontinuing those that can increase bleeding prior to surgery
- Get appropriate sleep
- Exercise in preparation for your recovery and rehabilitation
- Perform daily quadriceps isometric exercises to prepare for after surgery
- Reduce alcohol intake (try to stop before surgery)
- Stop smoking (smoking increases complication)

What Is The Expected Pain With Total Robotic Knee Replacement?
Mako Robotic Total Knee Replacement Surgery performed by Dr. Buechel can be less painful than when done by other surgeons for several reasons. A comprehensive pain control process has been developed by Dr. Buechel to make the procedure as comfortable as possible. The first 2 days are generally very comfortable due to the anesthetic blocks he uses. Days 3 through 6 are the days that can be most uncomfortable, as the blocks start to wear off, but several medications and therapies are provided to reduce pain. A combination of NSAIDs, acetaminophen, narcotic medicine, a cold therapy device, a compressive leg sports sleeve and elevation for swelling control provides good pain control, however, Dr. Buechel’s pain control program includes all the following:
- He has his anesthesiologist provide you with a spinal anesthesia if possible and two blocks that give you great pain control after the surgery for 36 to 48 hours. He also places local anesthetic into the wound to provide you with even more pain control.
- He provides you with a knee cooling sleeve after surgery to reduce pain and swelling.
- A sports compression sleeve that Dr. Buechel will place on you in the office the day after surgery reduces swelling and pain.
- Elevation is part of his protocol, and along with the compression sleeve swelling is reduced which reduces pain.
- Dr. Buechel does not use a tourniquet which dramatically reduces pain after and during surgery, which allows for better bleeding control, reducing swelling and pain after surgery.
- The anesthesia team uses Dexamethasone IV steroid to reduce swelling after surgery and provide some increased pain control
- Before surgery, if you are taking prescription pain medications you should try to eliminate them as best as possible so that they can be more effective around the time of surgery.
Each person experiences pain differently, which is why we use so many different modalities to help minimize this pain and individualize medications according to each patient’s needs.
What Can You Expect During A Robotic Total Knee Replacement Surgery?
During your office visit, you should expect to provide a comprehensive medical and knee history for Dr. Buechel to discuss with you. You will have a physical examination by Dr. Buechel who will be able to determine all the functioning and painful parts of your knee and body, as well as how you currently walk and function. Dr. Buechel will review your x-rays with you to confirm the condition of your knee and explain why a knee replacement will help your condition.
During the operation, you will me the operating room staff and anesthesia team that will care for you during the surgery. You will be made comfortable on the operating room bed and kept warm with blankets and heating systems during the procedure. You will have an IV to provide you medications, fluids and for safety during the procedure. You will have the option to be awake or asleep with a spinal anesthetic, or you will definitely be asleep if you choose a general anesthetic.
Your surgical time will be approximately one hour give or take depending on your knee condition and body size. There is also time to get you set up and prepared for the operation, which includes anesthesia induction time, wake up time, getting your dressings on and x-rays completed before leaving the operating room.
Once the surgery is over, you will be brought to the recovery room where nurses will care for you during the recovery from your anesthesia. Then, depending on your health and planning, you will either be admitted to the hospital, or discharged to home after being seen by the therapy team.

What Is The Followup And Recovery Like For Total Knee Replacement Surgery?
The follow-up care and recovery for robotic total knee surgery starts in the hospital. Patients are managed by our medical and surgical team in the hospital during their stay. Physical therapists are a key part of getting patients up and mobile after surgery. Therapists participate in the care at the hospital and for several months after surgery in rehabilitation facilities, during home physical therapy, and in outpatient therapy programs.
Most patients start with a walker or crutches to help with getting around after surgery. Patients can fully bear weight on the leg the day of surgery and are encouraged to do so starting the very first day. In general, each person recovers differently and at their own pace, however, most patients are functional to go back to light duty work by about 4-6 weeks. By 12 weeks, patients start to feel like they are becoming more normal in there activities and are not restricted at this point. Most patients by 3 to 6 months are back to full activity but describe a stiffness and soreness when they first get going still. Most patients will tell you that they continued to improve over a long period of time and found that by 18-24 months they felt that they were maximally recovered.
Early in the follow-up care for total knee replacement patients the focus is on swelling control, pain control, achieving good wound healing and avoidance of infection, and a return of functional motion and activity.
Wound healing is critical and good nutrition & protein intake, supplementation with Vitamin C, and avoidance of smoking are important in wound healing optimization. Skin adhesives are used by Dr. Buechel to keep out bacteria, allow for showering right after surgery, and avoid having painful staples removed that leave unpleasant scaring.
Swelling management is a critical part of proper care following total knee surgery. Keeping the leg elevated when not walking or exercising after surgery for the first 2-3 weeks significantly reduces potential leg swelling along with the leg compression sports sleeve Dr. Buechel provides.
Office follow-up visits with the surgeon early on are for wound evaluation, swelling evaluation, range of motion checks, pain control discussions and to listen to and help with any issues that have arisen since the surgery. As the weeks and months pass, follow-up becomes more focused on function, strength and motion. As the years go by, interval examinations are done to evaluate for implant insert plastic wear and metal bone attachment to ensure the implants are stable.
Contact our orthopedic practice today to schedule your consultation with Dr. Buechel of Robotic Joint Center.